Apnea Hypopnea Index (AHI) is the key measure used to detect and grade sleep-disordered breathing. It represents the number of apneas and hypopneas you experience per hour and serves as a scale indicating whether you have sleep apnea and, if so, how severe it is. Generally, an AHI below 5 events per hour is considered normal. Explore treatment options and equipment at CPAP Discount Warehouse.
What is AHI?
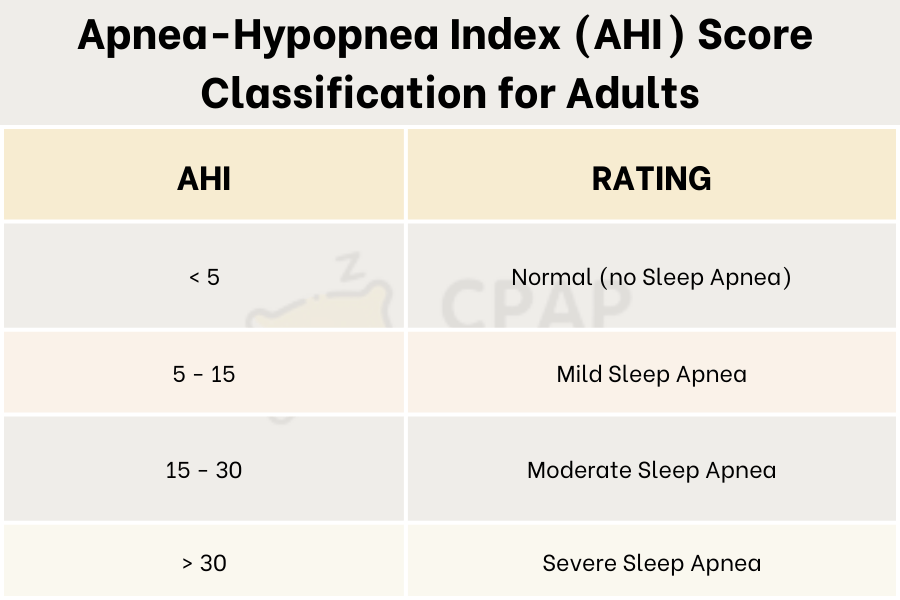
The apnea-hypopnea index (AHI) is the average number of times you stop breathing (apneas) or breathe shallowly (hypopneas) per hour of sleep. AHI sleep apnea scores categorize sleep apnea into a normal status when less than 5, mild between 5 to 15, moderate between 15 and 30, or severe if AHI is greater than 30; the higher the score, the more frequent the breathing disruptions. In summary, the severity of sleep apnea will be determined as follows: Mild sleep apnea: 5 ≤ AHI < 15; Moderate sleep apnea: 15 ≤ AHI < 30; Severe sleep apnea: AHI ≥ 30.
The AHI is a useful tool for diagnosing obstructive sleep apnea (OSA) and determining its severity. OSA is a common sleep disorder, and people with OSA experience multiple partial or complete obstructions of the airway during sleep, which are termed hypopneas and apneas, respectively. Additional symptoms may include loud snoring, gasping or choking, and excessive daytime sleepiness.

>>> Obstructive Sleep Apnea (OSA): Symptoms, and causes
How is the apnea-hypopnea index calculated?
Doctors usually determine the Apnea‑Hypopnea Index (AHI) during an overnight sleep study called a polysomnography which records brain waves, breathing, oxygen saturation, heart rate, and sometimes CO₂ levels. While most PSGs are performed in a sleep lab, simplified home-based versions are available.
AHI is determined by dividing the total number of apnea (complete breathing pauses) and hypopnea (partial airway obstruction) events by the total hours of sleep:
AHI= (Apneas+Hypopneas)/HoursofsleepAHI
For example, if an individual experiences 40 episodes over an 8-hour sleep period, their AHI would be 5, indicating mild sleep apnea. Monitoring AHI over time is crucial for assessing the effectiveness of treatments like CPAP therapy. As a key indicator of sleep apnea severity, AHI helps guide medical professionals in treatment adjustments and patient care.
What does AHI mean for sleep apnea?
The value in the AHI indicator shows the number of apneas and hypopneas a person experiences during one hour of sleep. Apnea is the cessation of breathing for more than 10 seconds during sleep. The AHI value or index indicates how often a person stops breathing within an hour. This index can then be used to determine how the breathing pattern can be controlled and regulated with CPAP therapy.
AHI scores categorize sleep apnea into a normal status when less than 5, mild between 5 to 15, moderate between 15 and 30, or severe if AHI is greater than 30; the higher the score, the more frequent the breathing disruptions.
Understanding the Apnea-Hypopnea Index for Adults and Children
The AHI is a key metric used to evaluate the severity of sleep apnea. It is determined by calculating the number of apnea (complete pauses in breathing) and hypopnea (partial reductions in airflow) episodes per hour of sleep. The AHI score correspond to different levels of OSA
The criteria for diagnosing sleep apnea in children differ slightly from adults due to their heightened sensitivity to breathing disturbances.
| AHI Classification for Adults | AHI Classification for Children | |
| Normal | < 5 episodes/hour | < 1 episode/hour |
| Mild Sleep Apnea | 5–15 episodes/hour | AHI 1–5 episodes/hour |
| Moderate Sleep Apnea | 15–30 episodes/hour | AHI 5–10 episodes/hour |
| Severe Sleep Apnea | > 30 episodes/hour | AHI > 10 episodes/hour |
>>>> What is Severe Sleep Apnea Symptoms? How do you treat it?
What is a normal AHI for sleep apnea?
If your AHI score is normal, it means you do not have obstructive sleep apnea. This means you experience fewer than five (<5) episodes of apnea per hour of sleep.
If you undergo a sleep study, your sleep specialist will determine whether your AHI is normal and what the next steps are. If you have a normal score, some sleep specialists aim for only 1-2 episodes per hour to achieve the best quality of sleep.
On the other hand, if you have a very high AHI, even a small reduction will significantly improve your sleep quality. For example, if your AHI is 75, reducing it to 50 will improve your sleep quality and make your breathing much more regular.
How Is AHI Measured?
Most often, AHI is determined during an overnight sleep study known as a polysomnogram. This test records multiple body functions while you sleep, including brain activity, heart rate, oxygen saturation, and breathing patterns. Though full sleep studies are typically conducted in dedicated sleep labs, simplified at-home versions may be available depending on your situation and symptoms.
While AHI is a central measure for diagnosing OSA, doctors often look at additional data to form a complete picture of your condition. One such measure is the Oxygen Desaturation Index (ODI), it tracks how often your blood oxygen levels drop significantly (usually for 10 seconds or more) over the course of an hour.
Another important factor, particularly in children, is the carbon dioxide (CO₂) level in the blood. Elevated CO₂ may indicate that breathing is consistently shallow or inadequate, even if no full blockage is detected. This can point to hypoventilation, a condition where airflow is limited over time.


– Dave Hurley, Verified Tester
>>> Sleep Apnea Home Study: When, Why, How, and Troubleshooting Tips
Treatment After a Moderate or Severe AHI Score
There are several treatment options you can pursue, regardless of whether your obstructive sleep apnea is mild or severe. If you have a mild sleep apnea-hypopnea index (SAHI), your doctor may recommend small lifestyle changes, such as quitting smoking or losing weight, to improve your symptoms. For patients with a higher AHI, there are several treatment methods that can keep the airways open, regulate breathing, and improve sleep quality.
Continuous positive airway pressure CPAP machine is the most popular and effective treatment method. The sleep apnea-hypopnea index can also be improved by using other devices to maintain airway pressure, such as bi-level positive airway pressure BiPAP machines or oral devices that keep the airways open during sleep.
Other treatment methods may include:
+ Surgical procedures (tissue removal, jaw repositioning, or even tracheotomy).
+ Treatment of comorbidities, such as allergies.
+ Changes in medication.
+ Additional oxygen supply.
+ Adaptive servo-ventilation (ASV) – a device for regulating airflow.

Causes of rising apnea-hypopnea index
If your nightly AHI readings start to rise above the recommended level, several factors may be contributing:
Mask leaks: If air escapes from your CPAP mask, you may not receive enough pressure to keep your airway open. The most common causes of mask leak are an ill-fitting mask, inadequate cleaning, or mouth leak. Mouth leak often occurs if you use a bilevel PAP device or if you naturally breathe through your mouth while using nasal pillows or a nasal mask. Addressing fit, maintenance, or mouth-breathing issues can usually correct the problem.
Mask-off events: Some people remove their mask during sleep, either consciously or unconsciously, due to discomfort or the unfamiliar sensation of wearing it. If your CPAP machine records these events or you suspect they occur, it is quite common. However, speak with your sleep specialist about strategies to minimise mask removal so you can maintain the full therapeutic benefit.
Alcohol, medications, or other substances: Drinking alcohol, taking sedatives, or using certain prescription or recreational drugs can increase AHI by relaxing the airway or affecting breathing patterns. Review any medications or substances with your doctor to see if they could be influencing your results and discuss safe adjustments if needed.
Central or complex sleep apnoea: A rising AHI may also indicate that, while CPAP effectively treats obstructive apnoeas, your brain is not consistently sending signals to breathe. This can result in central sleep apnea, which originates in the central nervous system rather than from a physical airway blockage. Most modern CPAP machines can detect central events, but if the cause of your increasing AHI is unclear, arrange a prompt review with your sleep physician or equipment provider.
FAQs
Why is my AHI so high?
There are three possible reasons for an increased AHI. The first is a mask leak. If your CPAP mask leaks, you will not receive the necessary air pressure to keep your airway open. This results in an increased AHI. Second, consuming alcohol, narcotics, and other drugs can increase obstruction and consequently increase your AHI. Third is development of central or complex sleep apnea
Is an AHI of 1.3 good?
Yes, an AHI of 1.3 falls well within the normal range of fewer than five events per hour, whereas a severe AHI is defined as more than 30 events per hour
What AHI score requires CPAP?
An AHI below 5 is normal. A score between 5–15 means mild sleep apnea, 15–30 is moderate, and over 30 is severe. Sleep experts usually recommend CPAP for people with moderate to severe sleep apnea (AHI of 15 or more). The goal of CPAP is to bring your AHI below 5 and help you breathe normally during sleep.
What does AHI 2.0 mean?
If your AHI is 2.0, it means you experience approximately two episodes of apnea or hypopnea per hour while you’re asleep.
Why does my AHI change?
It is normal for your AHI to vary within reasonable limits. However, if your AHI is stable and suddenly increases over the last few days or weeks, you should report this to your equipment supplier and/or sleep specialist.