Apnea definition refers to the temporary cessation of breathing. During this condition, the muscles involved in inhalation do not move, and the lung volume initially remains unchanged. Whether air flows between the lungs and the environment depends on the degree of airway obstruction. CPAP Discount Warehouse provides comprehensive information on the different types of apnea, their causes, symptoms, potential complications, and available treatments to help you better understand and manage this condition.
What does apnea mean?
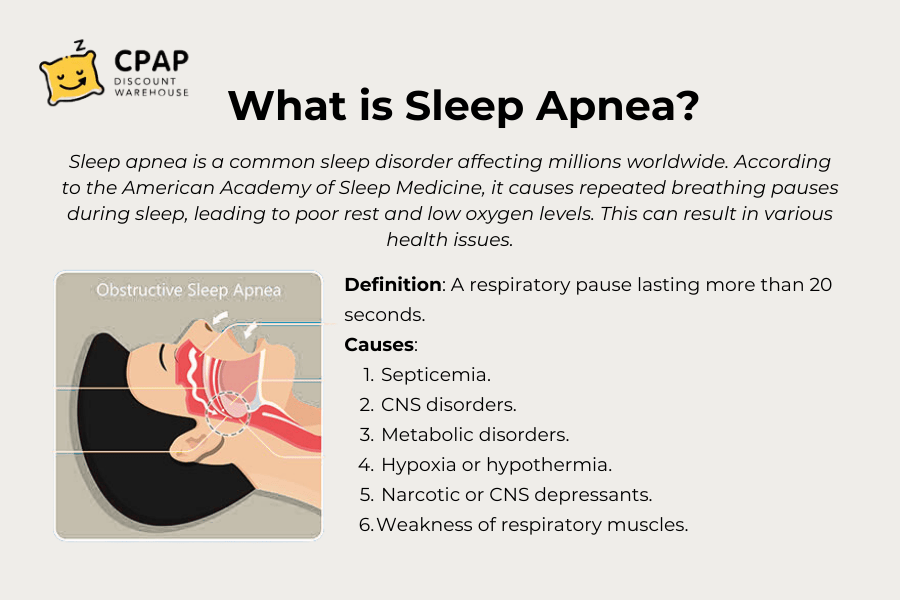
Apnea is defined as a temporary pause in breathing that occurs suddenly and without warning, lasting at least 20 seconds or more in full-term infants. During an episode, the muscles responsible for inhalation remain still, and lung volume does not change. While the term "apnea" is most commonly associated with sleep apnea, it can also refer to other conditions that lead to disrupted breathing. Understanding the various types of apnea, along with their causes, symptoms, potential complications, and treatment options, can help you identify and manage this condition effectively.
Sleep Apnea Definitions
-
Central Apnea: A condition where there is a lack of airflow and no inspiratory effort for a duration of 10 seconds.
-
Obstructive Apnea: A condition where airflow is blocked, but respiratory effort continues or increases for at least 10 seconds.
-
Hypopnea: A decrease in airflow of 30% or more, accompanied by a 4% or greater drop in oxygen saturation, lasting for 10 seconds.
-
RERA (Respiratory Effort-Related Arousal): A condition that does not meet the criteria for apnea or hypopnea but involves increasing respiratory effort over 10 seconds.
3 Types of sleep apnea
Obstructive sleep apnea (OSA): The most common type, occurring when the throat muscles relax, leading to a blockage that restricts airflow into the lungs.
Central sleep apnea (CSA): A condition where the brain fails to send the correct signals to the muscles responsible for breathing.
Treatment-emergent central sleep apnea (complex sleep apnea): A condition in which a person initially diagnosed with OSA through a sleep study develops CSA while undergoing treatment for OSA.
What Causes Apnea?
Some common causes include:
- Neurological factors: Conditions like head injuries or strokes that impact the brain's ability to regulate breathing.
- Central control issues: The brain fails to send proper signals to the respiratory system.
- Neuromuscular disorders: Diseases affecting the nerves and muscles involved in respiration.
- Airway obstruction: Blockages caused by choking on food or foreign objects.
- Cardiac arrest: A sudden loss of heart function that can lead to respiratory failure.
- Medications and substances: Certain drugs, including opioids and anesthetics, can suppress the respiratory center, leading to shortness of breath.
- Metabolic imbalances: Conditions like metabolic alkalosis that disrupt normal breathing patterns.
Symptoms of obstructive and central sleep apneas
The primary symptoms associated with both obstructive and central sleep apnea include:
- Loud snoring.
- Morning headache.
- Gasping for air during sleep.
- Awakening with a dry mouth.
- Difficulty paying attention while awake.
- Difficulty staying asleep, known as insomnia.
- Excessive daytime sleepiness, known as hypersomnia.
- Episodes in which you stop breathing during sleep — which would be reported by another person.
- Irritability.
>>> Learn more about: Sleep Apnea Symptoms And Treatments
When to See a doctor
While loud snoring may be a sign of a serious condition, not everyone with sleep apnea snores. Consult your healthcare provider if you experience symptoms of sleep apnea. Additionally, discuss any sleep-related issues that cause persistent fatigue, daytime drowsiness, or irritability.
How Is Apnea Diagnosed?
Diagnosing apnea generally requires a medical assessment and may involve various tests, including:
-
Pulmonary function tests: Evaluating lung performance and airflow.
-
Sleep studies: Monitoring breathing patterns, oxygen levels, and other factors during sleep.
-
Imaging tests: Using scans to detect structural abnormalities that may contribute to apnea.
During the diagnostic process, doctors may use several methods, such as:
-
Apnea monitors: Devices, often used in hospitals or for infants at home, that detect pauses in breathing.
-
Blood gas analysis: Measuring oxygen and carbon dioxide levels in the blood to assess respiratory efficiency.
-
Clinical evaluation: Examining reflexes, responses, and potential underlying neurological or metabolic conditions.
Treatment and Management of Sleep Apnea
Effectively addressing sleep apnea begins with understanding its causes. Below are common treatment approaches:
-
Medication: Prescription drugs like caffeine or theophylline may be used to stimulate breathing, particularly in premature infants.
-
Surgical Intervention: In some cases, surgery may be required to correct structural abnormalities that contribute to sleep apnea.
-
Lifestyle Modifications: Maintaining a healthy weight, avoiding alcohol, and quitting smoking can help reduce apnea episodes.
-
Respiratory Therapy: Treatments such as continuous positive airway pressure (CPAP) are widely used to keep the airways open during sleep.
-
Emergency Interventions: In critical situations, techniques like the Heimlich maneuver for choking or cardiopulmonary resuscitation (CPR) for respiratory arrest can be lifesaving.
-
Mechanical Ventilation: In severe or prolonged cases, ventilators may be necessary to assist with breathing.
-
Behavioral Therapy: Breathing exercises and retraining techniques may be recommended, particularly for voluntary apnea or breath-holding episodes in children.
The choice of treatment depends on the underlying cause and severity of the condition, ensuring that the approach is both effective and tailored to the individual’s needs.
Complications of apnea
Sleep apnea is a serious medical condition that can lead to various health issues.
|
Complications of Obstructive Sleep Apnea (OSA) |
Daytime fatigue |
|
High blood pressure or heart diseases |
|
|
Type 2 diabetes |
|
|
Metabolic syndrome |
|
|
Complications with medicines and surgery |
|
|
Liver problems |
|
|
Bed partner sleep disruption |
|
|
Complications of Central Sleep Apnea (CSA) |
Fatigue |
|
Cardiovascular problems |
When sleep apnea increases in severity, it can cause a drop in air pressure within the airway, leading to further breathing difficulties. If untreated sleep apnea persists, it can increase the risk of serious complications, including cardiovascular problems. Studies show that losing weight can significantly reduce symptoms, as excess weight contributes to airway obstruction. However, without proper management, sleep apnea can increase your risk of developing conditions such as high blood pressure, heart attack, and even heart failure over time.
Associated Conditions
Sleep apnea
Sleep apnea is a condition where breathing repeatedly stops during sleep. This happens either due to a blocked airway (obstructive sleep apnea) or the brain not sending signals to breathe (central sleep apnea). It can cause poor sleep, daytime tiredness, and increase the risk of heart and metabolic problems. Common signs include loud snoring, gasping for air, and morning headaches.
Hyperventilation
Hyperventilation is fast or deep breathing that removes too much carbon dioxide from the blood. It can cause dizziness, tingling in the fingers and lips, shortness of breath, and chest pain. Common triggers include anxiety, panic attacks, or medical conditions. People may feel like they can't breathe properly, sometimes leading to breath-holding or apnea.
Apneic oxygenation
Apneic oxygenation is a technique used to maintain oxygen levels when a person temporarily stops breathing. It involves giving extra oxygen, usually through a nasal cannula, to prevent oxygen loss. This method is especially useful during procedures like intubation, helping keep oxygen levels stable while the airway is blocked.
FAQs
What is the meaning of apnoea?
A medical condition that temporarily disrupts breathing, often occurring during sleep, known as sleep apnea.
What happens when you have apnea?
Obstructive sleep apnea happens when the muscles supporting the soft tissues in the throat, including the tongue and soft palate, temporarily loosen. This relaxation causes the airway to become restricted or completely blocked, briefly interrupting breathing.
What does apnea mean in medical terms?
Pertaining to apnea, a condition where an individual, whether a sleeping adult or an infant, experiences an involuntary and temporary pause in breathing. In individuals with apneic episodes, the muscles of the tongue or soft palate may become overly relaxed and collapse against the throat, obstructing airflow.
What is the main cause of apnea?
Central Sleep Apnea (CSA) caused by disruptions in how the brain controls breathing during sleep. Obstructive Sleep Apnea (OSA) caused by factors that obstruct airflow in the upper airways during sleep. For example, the tongue may fall back and block the airway.
Conclusion
Understanding the definition of apnea and its various types is crucial for maintaining good health. Recognizing its symptoms, causes, and risk factors enables early detection and timely treatment, helping to minimize the higher risk associated with the condition.